
| Teaching Round | |
| Polycystic Ovarian Syndrome: a Management Dilemma | |
| Pikee Saxena, Aruna Nigam
Department of Obstetrics and Gynaecology, Lady Hardinge Medical College & Smt. Sucheta Kriplani Hospital, New Delhi, India
Corresponding Author: Dr Pikee Saxena, Assistant Professor, Department of Obstetrics & Gynecology, LHMC & SSKH, New Delhi- 110001. E-mail: pikeesaxena@hotmail.com
A 24 years old married female presented with complaints of inability to conceive for last 3 years. She gives history of irregular menstrual cycles (3-5 days/45-60 days), increased hair growth over the face & breasts & acne for last 6 yrs. She also gives history of weight gain of 8-10 kg over last 5-6 years. Her coital history is normal and there is no history of discharge from breasts or vagina. There is no history suggestive of tuberculosis, thyroid disorder, diabetes mellitus or hypertension. Her mother is obese and diabetic. Her maternal aunt died of uterine malignancy 2 years back. On general physical examination:, Ht – 152cm; Wt – 68kg; Waist circumference – 38cm; Hip circumference – 40cm; Waist / Hip circumference – 0.95; BMI – 29.43, Acne +; Hirsutism + with Ferriman Gallway Score of 13; No acanthosis nigricans. BP – 130/90 mm of Hg ; Pulse- 86 per minute, regular. No abnormality was detected on systemic and gynaecological examination. What is the probable diagnosis? Polycystic ovarian syndrome (PCOS). It is the commonest cause of anovulatory infertility with acne, hirsutism and obesity. Family history of diabetes and uterine malignancy is also pointing towards a hereditary link of hyperoestrogenic condition which is seen in this disease. What are the criteria for diagnosing PCOS? According to the revised 2003 diagnostic criteria of PCOS [1], the presence of any two out of the following three suffices for the diagnosis of PCOS: 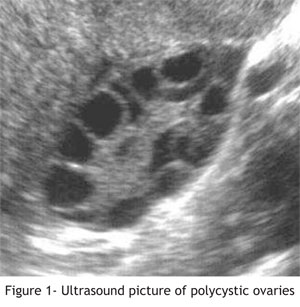 1. Oligo- or anovulation 2. Clinical and/or biochemical signs of hyperandrogenism 3. Polycystic ovaries on ultrasound scan, defined as the presence of 12 or more follicles in each ovary (with one ovary being sufficient for the diagnosis), measuring 2-9 mm in diameter, and or increased ovarian volume (>10mL), and/ exclusion of other etiologies. What are the other causes of multiple ovarian cysts on ultrasonography (USG)? How can polycystic ovaries be differentiated from multicystic ovaries? Any condition which leads to chronic anovulation can give rise to multiple small cysts in the ovary i.e. congenital adrenal hyperplasia, virilizing tumors and Cushing's syndrome. The typical findings on sonogrpahy are described above and the increased density of ovarian stroma differentiates polycystic ovaries from multicystic ovaries. Multiple small cysts in a single plane of the ovary on USG is considered most characteristic of polycystic ovaries, particularly if these cysts are peripherally arranged in the so-called "pearl necklace" configuration (Figure1). What is the clinical presentation in PCOS? The clinical spectrum of patients with PCOS varies from mild hyperandrogenism with apparently regular menses to more severe disorder with manifestations of menstrualdisorders, hyperandrogenism causing hirsutism, acne and virilisation (rarely), anovulatory infertility, obesity and other metabolic disorders at the other end of the spectrum [2]. These patients may present at any time during reproductive age group and because of varied symptoms, they may present to a gynaecologist, reproductive endocrinologist, physician, dermatologist or a dietician. What is the pathophysiology of PCOS? The basic pathology lies in dysregulation of enzyme cytochrome P-450-17- α hydroxylase which is present in ovaries and adrenals and has a genetic link. This enzyme system catalyses the activities of two enzyme systems i.e. 17- hydroxylase and 17, 20 - lyase resulting in hyperandrogenism [3,4]. PCOS is also associated with hyperinsulinemia and insulin resistance [2]. High insulin level probably acts at multiple sites like ovary, liver, hypothalamopituitary axis and the adrenal cortex. In the ovary and adrenals it increases androgen production. In liver it reduces the production of insulin growth factor binding protein-1 (IGBF-1) and sex hormone binding globulin (SHBG), which further increases free androgen levels. High androgen levels prevent development or maturation of follicles producing polycystic ovaries, potentiates luteinizing hormone (LH) and suppresses follicle stimulating hormone (FSH). Under LH influence, cholesterol is converted to androstenedione in the theca cell which is then transferred to the granulosa cell to form oestrone and oestradiol [3]. Excess oestrogen increases obesity and insulin resistance and thus a vicious cycle is formed. How will you work up a patient of PCOS? Careful clinical history, physical examination and laboratory investigations in these patients can clinch the diagnosis. Salient points on history [4] • History of mode of onset and progress of signs and symptoms. • Age of onset and the pattern of past and present menstruation- irregularity/oligomenorrhea /amenorrhea. • Previous investigations and treatment received and the results thereof. • Personal history- occupation, life style, history of low birth weight or precocious puberty. • Ethnic origin and family history of similar problem and of diabetes mellitus. Salient points on physical examination [4] • Height, body weight, body mass index (BMI) • Pulse rate, Blood pressure, • Waist and hip circumference • Signs of hyperandrogenism- hirsutism and its distribution (Ferriman Galway score); acne; pubic hair pattern; clitoral enlargement. • Hyperpigmentation, particularly on the back and sides of the neck, axillae, skin folds and pressor points. • Breasts- lobule-alveolar development which is less in case of chronic anovulation; galactorrhoea Laboratory investigations [4] • Pelvic ultrasonography (transabdominal & transvaginal), especially for polycystic ovaries and stromal hypertrophy. Endometrial hyperplasia should be evaluated. • Glucose tolerance test - measure glucose and insulin at least at ‘0’ hour (fasting) and at 2 hours after 75 g glucose given orally. • Fasting levels of FSH, LH, prolactin, TSH, testosterone, androstenedione, 17α OHprogesterone & DHEAS, on any of day 3 to 5 after natural or progestin withdrawal bleeding. • Lipid profile What are the treatment protocols for managing infertility in PCOS? ACOG (2002) recommends stepwise approach for ovulation induction in PCOS 1. Weight loss by exercise and diet control: If BMI 2 >30 kg/m 2. Clomiphene citrate (CC) for ovulation induction 3. CC + corticosteroids if DHEAS > 2 μg/ml 4. CC + Metformin (insulin sensitiser) 5. Low dose FSH injection 6. Low dose FSH injection + Metformin 7. Ovarian drilling 8. In Vitro Fertilisation What are the long term implications of PCOS? Young women with PCOS should be counselled regarding the possible long-term risks associated with this condition [5,6]. These are- Definite: Type 2 diabetes (15%), Impaired glucose tolerance (IGT) (18 - 20% ), Dyslipidemia (Hypercholesterolemia with diminished HDL and increased LDL), Endometrial cancer (OR 3.1, 95% CI 1.1 -7.3) Possible: Hypertension, Cardiovascular disease, Gestational diabetes mellitus, Pregnancy-induced hypertension Which are the two different distinct phenotypes of PCOS patients? There are two phenotypes of PCOS- Insulin resistance (IR) Phenotype of PCOS- Associated with abdominal obesity, Acanthosis Nigricans, hirsutism and they are resistant to CC; and PCOS without IRThese patients are lean, euinsulinemic/ euglycemic and have enhanced ovarian sensitivity to insulin (although no hyperinsulinemia exists). Which tests can be used to determine insulin resistance? For the measurement of insulin resistance, the following methods have been used [4]: a) The euglycemic insulin clamp b) The minimal model c) Fasting blood insulin level d) Fasting glucose/insulin ratio The first two are much more elaborate research methods and not suitable for wider clinical use. From a clinical perspective, the most practical way and sensitive indicator of assessing insulin resistance would seem to be the measurement of insulin in plasma in the fasting state and/or after a glucose load. In the majority of the patients, blood level of fasting insulin is normal, but after glucose load it shows exaggerated response. References
|