| |
 |
| Case Report |
| |
|
| |
Shankar Acharya, Gurdeep Singh Ratra
Department of Orthopaedics, Sir Ganga Ram Hospital, New Delhi.
Corresponding Author: Dr. Shankar Acharya, 38, Engineer’s Enclave, Pitampura, New Delhi. 110088. E mail: shankaracharya29@gmail.com
Abstract
We present a case of chondrosarcoma D12 vertebra in a patient with ankylosing spondylitis, treated with vertebrectomy (marginal excision) and single stage combined anterior & posterior decompression, fixation and fusion. Patient has been symptom free at 3 year follow up.
Keywords: Ankylosing spondylitis, Pseudoarthrosis, Chondrosarcoma.
|
Introduction
Chondrosarcoma is the second most common primary malignant bone tumor, however, chondrosarcoma of the spine is a relatively uncommon entity [1]. A case report of chondrosarcoma D12 vertebra in a patient with ankylosing spondylitis, treated by vertebrectomy (marginal excision) and single stage combined anterior & posterior decompression, fixation and fusion is being reported. A tumor arising de novo in a pseudoarthrosis in Ankylosing Spondylitis makes it a hitherto unreported unique case.
Report of case
A 63 year old male, diagnosed ankylosing spondylitis for over 20 years, presented with complaints of severe pain in the mid-back region for 15 years. He had taken irregular treatment for his backache and for ankylosing spondylitis. His previous x-rays showed features of ankylosing spondylitis with osteoporosis and pseudoarthrosis at D11-D12 level. He used a hyperextension (A.S.H.) brace intermittently. In the last 15 days, his pain had increased and he developed weakness in both lower limbs. and radicular thoracic girdle pain. There was no history of trauma or presence of constitutional symptoms.
Clinical examination revealed tenderness over dorsolumbar region. Power in both lower limbs was grade 3/5 and bilateral knee and ankle jerks were absent; plantars were equivocal.
Blood investigations were normal, except for an elevated ESR (64mm/1st hour). Prostate specific antigen (PSA) was normal and myeloma screening was negative.
X-ray showed lytic lesion eroding D12 vertebra with fracture through D11-D12 in an ankylosed spine.
CT Scan with three—dimensional reconstruction was done, which showed an osteolytic destructive lesion (Fig.1) with sclerosed margins involving the superior end plate and D12 vertebral body and D11 inferior end plate with fracture line extending into the posterior arch elements, likely to represent a type III Anderson lesion.

Fig. 1: Preoperative CT slice.
===========
CT guided FNAC was suggestive of low-grade chondrosarcoma.
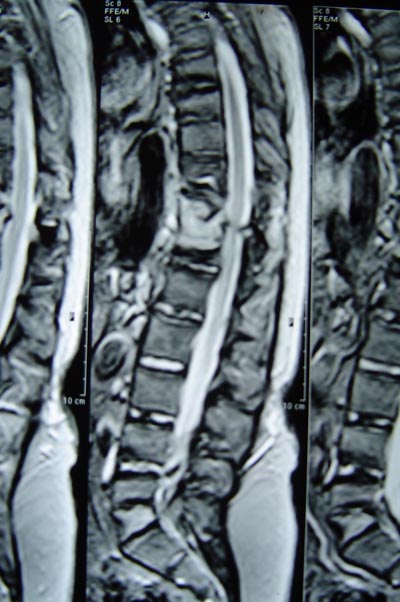
On MRI, whole D12 vertebral body showed increased signal intensity (Fig.2) with expansion and destruction of cortical margin with cord compression at D11-D12 level.
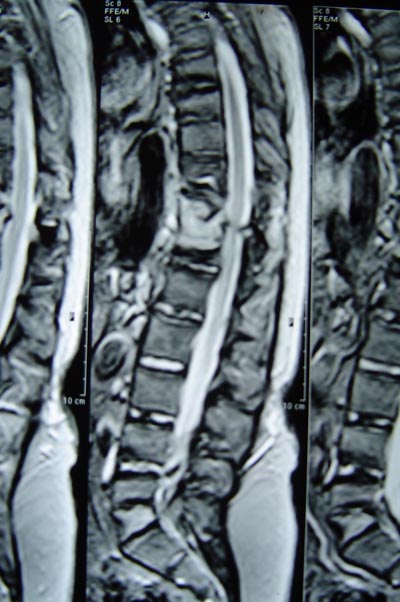
Fig. 2: Preoperative MRI.
Technetium bone scan showed no evidence of bony metastases. Ultrasound abdomen and CT chest were normal.
========
A single stage posterior and anterior decompression and fixation was performed. Posteriorly, pseudoarthrosis with fibrous tissue was found at D11-D12 level. Laminectomy and decompression was done and pedicle screws were put on both sides at D9, D10 above and L1, L2 below and fixed with contoured rods (USS). Bone graft mixed with synthetic tricalcium phosphate graft (chronos) was put posterolaterally on both sides. Anteriorly, transthoracic approach was employed through the 10th rib bed. D12 vertebra was found to be completely destroyed and replaced with white cheesy material. There was erosion of inferior end plate of D11. All abnormal looking tissue was removed till healthy bleeding bone was seen. Excised tissue was sent for biopsy. Expandable cage (syncage) was used to bridge the defect (Fig.3). Around the cage, harvested bone and rib graft was put and chest closed over an intercostal drain tube.

Fig. 3: Postoperative X-Ray.
Post-operatively, the patient developed chest infection with compromised oxygen saturation. He needed ICU care and was intubated and later tracheostomized due to reduced lung compliance. Chest infection gradually settled and patient improved to power grade 5/5 with relief of pre-operative pain.
==========
Biopsy revealed cartilaginous tumor with widespread necrosis. Tumor cells showed prominent pleomorphism and spindle shaped appearance in focal areas. Final diagnosis was put as ‘Chondrosarcoma – moderately differentiated consistent with grade II’.
There has been no radiological or clinical evidence of recurrence of the tumor at 3 year follow-up.
Discussion
Chondrosarcoma is the second commonest primary malignant bone tumor [1], but chondrosarcoma of the spine is relatively rare. Chondrosarcoma spine is most commonly found in the thoracic spine [2]. It has been reported to have a higher incidence in patients less than 21 years of age with a male preponderance [3].
The treatment of chondrosarcoma is surgical excision. Surgical cure of chondrosarcoma spine is considered to be uncertain, as complete removal is usually difficult and may lead to local recurrence. Role of radiotherapy and chemotherapy is questionable [4].
During the pre-operative planning, the Weinstein-Boriani-Biagini (WBB) system [5] and the scoring system of Tomita, Kawahara et al [6] were used. The WBB system [5] divides a vertebra into twelve zones (1-12) in a clock face arrangement and into five tissue layers (A-E), from superficial paraspinal soft tissues to intraspinous extra-dural and finally intraspinous intradural. The tumor in the present case was extending from zone 3-10 and layers A-D.
Tomita, Kawahara et al [6] described a scoring system with prognostic score 2-10 based on three factors: 1) Grade of malignancy (slow growth 1 point; moderate growth 2 points; rapid growth 4 points), 2) Visceral metastasis (no metastasis 0 points; treatable 2 points; untreatable 4 points), 3) Bone metastasis (solitary 1 point; multiple 2 points). Surgical strategy depends on the total score. The present case scored 3 on this system.
Both these systems indicated an anterior surgery with marginal excision of the tumor. So, it was decided to fix the pseudoarthrosis posteriorly and do an anterior vertebrectomy.
Thompson and Turner-Warwick classified chondrosarcomas into three types [7]:
Grade I – Low grade, well-differentiated tumor with increased number of cartilage cells and well-defined matrix. 10-year survival rates after treatment – 71-83%.
Grade II - Average grade with less matrix and increased cellularity. Cells vary in size and shape. 10-year survival rate– 33%.
Grade III - High-grade tumor with anaplasia, mitosis and rare islands of cartilage. It is similar to osteosarcoma. Only 1 out of 10 patients survived after 3 years in this group.
Grade III tumors have been found to metastasize in 70% cases, whereas grade I tumors are unlikely to metastasize [8]. In the present case, the final biopsy report showed the tumor to be grade II.
In ankylosing spondylitis, an acute fracture can go undetected and may proceed to non-union and pseudoarthrosis, which presents radiographically as disco-vertebral erosions and bone destruction. This is referred to as the Anderson lesion. These lesions are further classified into type I (anterior lytic defect), type II (irregular central and peripheral lytic area) and type III (true pseudoarthrosis involving all three columns).
A possible hypothesis for the occurrence of chondrosarcoma in this case is an abnormal proliferative response of the chondrocytes recruited at the pseudoarthrosis site as part of the natural repair process.
Literature search shows many papers on destructive lesions and pseudoarthrosis in cases of Ankylosing Spondylitis [9,10]. While many cases mimicked discitis/ inflammation and even tuberculous infection, the definitive diagnosis in all cases was just a local pseudoarthrosis with fibroblastic proliferation. There is, to our best of knowledge, no reported case of a malignant tumor arising de novo in a pseudoarthrosis in Ankylosing Spondylitis.
Key Points
- Ankylosing spondylitis is a chronic systemic inflammatory rheumatic disease, primarily affecting the axial skeleton of which sacroilitis is the hallmark.
- Chondrosarcoma is the second most common primary malignant bone tumour, however, chondrosarcoma of the spine is rare.
- Chondrosarcoma arising de novo in a pseudoarthrosis of D12 spine in a case of Ankylosing Spondylitis is a unique combination.
|
References
-
Camins MB, Duncan AW, Smith J, Marcrove RC. Chondrosarcoma of the Spine. Spine 1978, 3:202-9.
-
Torma T. Malignant Tumors of the Spine and Spinal Extradural Space: A Study Based on 250 Histologically Verified Cases. Acta Chir Scand (Suppl) 1957, 225: 1-176.
-
Huvos AG. Chondrosarcoma in the Young: A Clinicopathological Analysis of 79 Patients Younger Than 21 Years of Age. Am J Surg Pathol 1987 Dec., 11(12): 930-42.
-
Evans HL, Ayala AG, Romsdahl MM. Prognostic Factors in Chondrosarcoma of Bone. Cancer 1977, 40: 818-31
-
Boriani S, Weinstein JN, Biagini R. Primary Bone Tumors of the spine – Terminology and Surgical staging. SpineMay 1997, Vol. 22 (9):1036-1044.
-
Tomita K, Kawahara N, Kobayashi T et al. Surgical strategy for spinal metastasis. SpineFeb 2001, Vol. 26(3): 298-306.
-
Thompson AD, Turner-Warwick RT. Skeletal Sarcomata and Giant Cell Tumor. J Bone Joint Surg 1955, 37-B: 266-303.
-
Harwood AR, Krajbich JI, Fornasier VL. Radiotherapy of Chondrosarcoma of Bone. Cancer 1980, 45: 2769-77.
-
Arnold MH, Brooks PM, Ryan M, Francis H. A destructive discovertebral lesion: septic discitis, ankylosing spondylitis or rheumatoid arthritis? Clin Rheumatol 1989 Jun; 8(2): 277-81.
-
Cawley MI, Chalmers TM, Kellgren JH, Ball J. Destructive lesions of vertebral bodies in Ankylosing Spondylitis. Ann Rheum Dis 1972 Sep; 31 (5): 345—58.
|
|
|