
| Teaching Round | |||
| Backache in a Diabetic Male: An Underdiagnosed Aetiology | |||
| *Nirupam Prakash, **Shweta Saxena
*Department of Posts, Lucknow, **HAL Hospital, Lucknow
Corresponding Author: Dr. Nirupam Prakash 41-42, Qaiserbagh, Lucknow-226001. E mail: nirupamprakash@yahoo.com
A 53 years male, known case of type 2 diabetes and hypertension for the last 5 years on regular treatment presented with complaints of backache and stiffness on bending forwards and sideways for the duration of last 6 months. On examination his vital statistics were pulse of 68/min and B.P. of 138/82mmHg right arm supine. His body mass index 2 was 27.9 kg/m . Systemic examination was essentially normal. Examination of the spine revealed local tenderness over the lower thoracic and lumbar spine. There was limitation of movement of forward and lateral flexion of the spine. The curvature of the spine was normal and there was no obvious swelling. No tenderness over the peripheral and sacroiliac joint was observed. Investigations revealed that the patient had a normal haemogram and ESR of 14 mm at the end of first hour (Westergren). His blood sugar levels were: fasting-106 mg/dl and postprandial of 165 mg/dL. He had a glycosylated haemoglobin of 6.7%, urea 28 mg/dL, creatinine 0.9 mg/dL and uric acid of 4.7 mg/dL. His serum calcium and phosphate were 9.2 mg/dL and 3.9 mg/dL, respectively. His alkaline phosphatase was 44 U/L and lipid profile showed total cholesterol 230 mg/dL, LDL 157 mg/dL, HDL of 41 mg/dL and triglycerides of 154 mg/dL. TSH levels were 1.75 U/L. HLA B27 was negative. His lumbosacral spine X rays are shown in Figure 1. What are the radiological findings (Figure 1)? What are the causes of low backache? Low backache commonly can arise from the muscles (lumbarsprain/strain), nerves-lumbar radiculopathy and nerve compression/irritation and from bone/joint conditions. Various causes of low backache are enlisted in Table 1 [1]. At times, the pain may be referred from the abdominal organs in which case it is known as a “referred pain”. 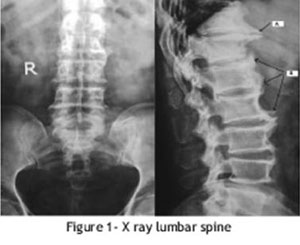 How can one differentiate inflammatory from non-inflammatory backache? Traditionally, five features distinguish the inflammatory back pain from non-inflammatory or mechanical back pain- 1. Age of onset below 40 years 2. Insidious onset 3. Duration > 3 months before medical attention is sought 4. Morning stiffness 5. Improvement with exercise or activity Recently, proposed criteria for inflammatory backache in an adult ≤ 50 years old are- 1. morning stiffness > 30minutes 2. improvement with exercise but not with rest 3. awakening from backache during the second half of night 4. alternating buttock pain Ankylosing spondylitis is the classical prototype of disease with inflammatory backache. His lumbo-sacral spine radiographs showed large osteophytes arising from the contiguous surfaces of D11 and D12 vertebrae (pointer arrow A). The lateral view of dorsolumbar spine showed continuous flowing ossification (“flowing wax” appearance) on the anterior surface of L1-4 vertebrae bridging across the intervertebral spaces (pointer arrows B). Disc space was well maintained and there were no findings suggestive of sacroiliac joint sclerosis or facet joint ankylosis. A diagnosis of Diffuse Idiopathic Skeletal Hyperostosis (DISH) was made. A less likely diagnosis could be Degenerative spondyloarthritis although the age is a factor against it. What radiological features distinguish DISH from ankylosing spondyltitis and spondylosis? The intervertebral spaces are preserved in DISH visà- vis spondylosis and the sacroiliac and apophyseal joints appear normal in DISH unlike ankylosing spondylitis which has sacroilitis and apophysitis. What are the characteristics of DISH? What is its relation to diabetes? Diffuse idiopathic skeletal hyperostosis (DISH), also known as “Forestier disease”, is considered to be a degenerative type of arthritis. It is a disease characterized by exuberant ossification of ligaments (enthesopathy) in both axial & appendicular skeleton. The disease begins early at around 20 – 40 yrs of age when there is ossification of tendinous attachments to bony projections like the calcaneum, patella and olecranon and diagnosis is often missed. The disease manifests after a couple of decades when there is involvement of the spine with florid flowing ossification seen on the anterolateral aspect of dorsal spine. Pathogenesis is not clearly understood. Factors implicated in causation are hyperinsulinemia with or without diabetes, hypertension, obesity, dyslipidemia & hyperuricemia[2,3,4]. Most common presentation is stiffness in back (dorsolumbar region) and localized back pain. The diagnosis is based on radiological features (Resnick and Niwayama) which are [5]: 1. flowing ossification along the anterolateral aspect of at least 4 contiguous vertebrae; 2. the preserved disk height, with absence of significant degenerative changes (marginal sclerosis in vertebrae) 3. absence of any significant facet-joint ankylosis, sacroiliac erosions, or intra-articular osseus fusion.
It is a less sought for disease and hence underreported. Complaints are non-specific and commonly ignored but have a high associated morbidity. Radiographic images may be confused with Ankylosing spondylitis but there is no sacroiliac involvement or facet joint ankylosis. Diagnosis is mostly late in course of disease when there is florid ossification of the spinal ligament, hence there is limited scope of drugs. Large osteophytes may cause radicular or cord compression and may be complicated with osteophytic fractures. Often large osteophytic spurs in cervical spine may be a cause of difficult intubation during surgery, failed endoscopic procedures and dysphagia. Therefore, DISH should be specifically sought for in individuals presenting with backache and stiffness with coexistentdiabetes, hypertensionor atherosclerotic vascular disease not only to limit the associated morbidity but also because it may antedate the occurrence of these disorders. What is the management of DISH? Although there is no definite cure for DISH, the primary aim is to provide symptomatic relief, which at times may not even be required (in asymptomatic individuals). Acetaminophen and non-steroidal antiinflammatory drugs are of use and may limit inflammation and further worsening. Corticosteroid injections can be used for severe pain. Physiotherapeutic exercises can reduce the stiffness so very characteristic of DISH. It can also help improve the range of movements of joints and improve productivity. Surgical intervention is restricted to patients who have complications viz. to remove bony spurs in the enck causing nerve root compression or dysphagia and to relieve pressure on the spinal cord caused by DISH. Patient was advised proper control of weight, life style modification and physiotherapeutic exercises along with Naproxen 250 mg BD as an antiinflammatory analgesic agent.
References
|